Metastatic Cancer
Oligometastatic Disease: An Overview
November 28, 2023
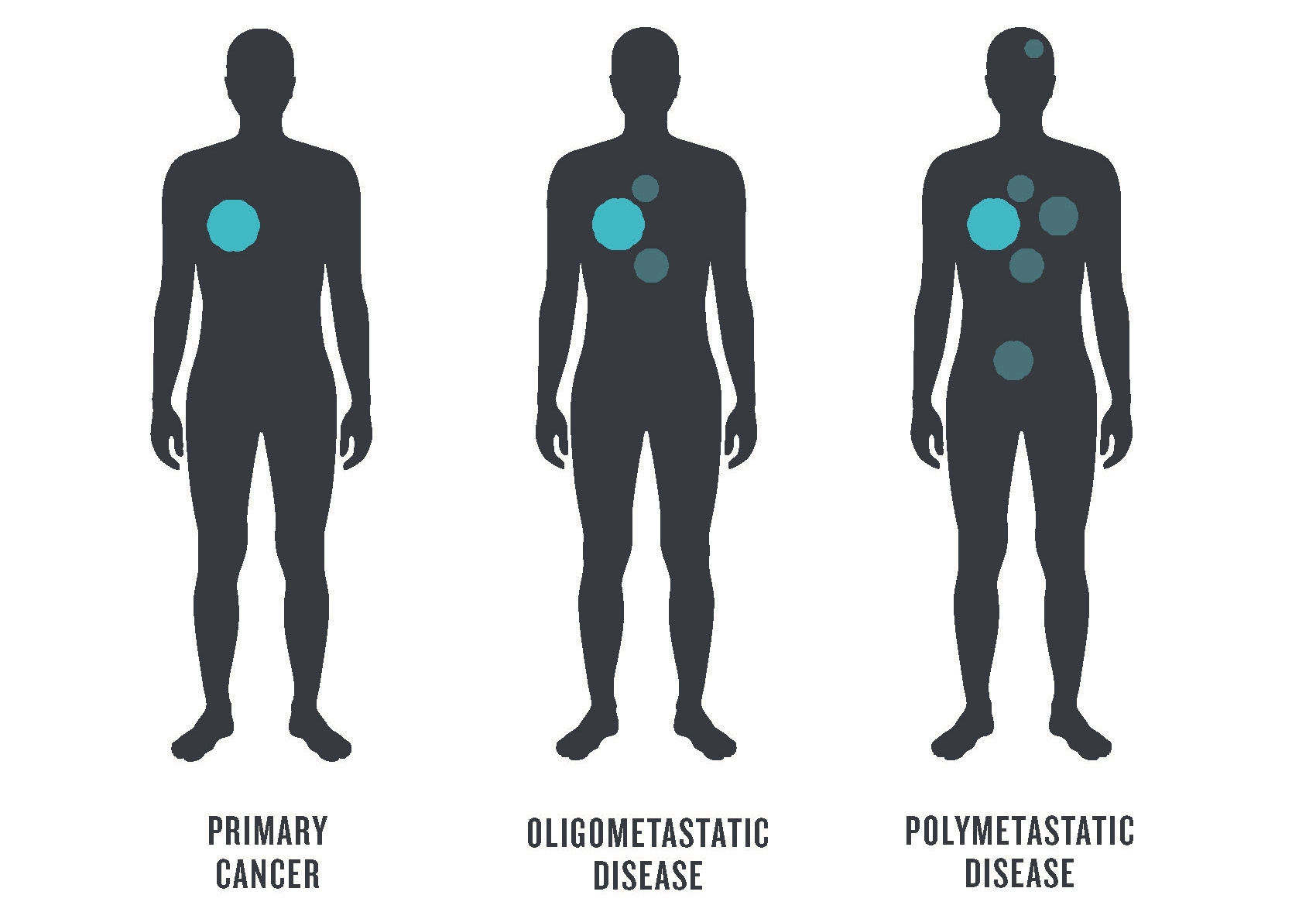
For patients battling cancer, little is more important than knowing exactly where they stand in the course of the disease. When a malignant tumor spreads from its original location to additional sites in the body, this means the disease has “metastasized.” If the disease has spread to many locations, this is sometimes termed polymetastatic disease. However, there is an intermediate stage, when the cancer has spread to a few, as opposed to many, regional sites—this is known as oligometastatic disease.
An evolving definition
Meaning “few” in ancient Greek, oligo is the basis for “oligometastatic.” A precise, agreed-upon definition of this clinical term has not been achieved, however. While MD Anderson indicates that oligometastatic cancer involves fewer than five sites,1 one recent study indicates there may never be an exact cutoff.2
The concept of the oligometastatic intermediate state of cancer, introduced almost 30 years ago,3 is gaining momentum as some patients are benefitting from localized surgery or radiation therapy of the metastasized sites.
Questions remain, however. Is the distance of the metastases from the primary tumor a factor? Does it depend on the type of cancer? On the size of the metastases and their location? On the physician’s capacity to treat them…or on the patient’s prognosis? Given these issues, the definition of oligometastatic disease could actually vary by patient.
The diagnosis of oligometastatic disease is also limited in that it is largely based on medical imaging as opposed to an analysis of processes that occur at a cellular level.4 Thus, the diagnostic criteria are visual, i.e., the number of metastases and the extent of disease visualized.
Potentially important variables that are not part of the criteria include cellular and molecular characteristics of the tumors, as well as kinetic measures of the disease (tumor volume or doubling times, for example). It is, therefore, difficult to predict why some patients with oligometastatic disease may experience long-term disease control, while others rapidly progress to more widespread metastasis.
Among the many attempts to define “oligometastatic” is “a state where the full metastatic potential has not yet been realized.”5 This definition has an encouraging implication as it suggests a spatially limited disease that, while challenging, may be amenable to treatment.
In order to make concrete progress, novel defining criteria and a more in-depth understanding of the disease biology and kinetics has to be formulated.
Findings from clinical trials
Clinical trials undertaken in many institutions and countries have played a key role in advancing the understanding and treatment of oligometastatic disease. These investigations have examined various treatment strategies that might improve outcomes for patients at this stage, especially for those with non-small cell lung cancer.6-8
The lessons learned from several clinical trials are summarized below.9
Despite a lack of consensus regarding the definition of oligometastatic disease, agreement on a standard of care is emerging. At present, aggressive local treatment appears to be the best approach as most randomized clinical trials indicate that patients derive benefits from ablative therapies and from treating all the lesions.10
Regarding the type of radiation therapy, the literature currently suggests that the best such tool is stereotactic ablative radiotherapy (also referred to as SABR) or stereotactic body radiotherapy (SBRT), treatments that provide an intense dose of radiation concentrated on a tumor, while limiting the dose to the surrounding organs.11 Although other modalities may have advantages in certain situations, the use of SBRT is currently backed by the most evidence, may be curative, and is well tolerated and cost-effective.12
Finally, further investigation is required to define the optimal timing of SBRT, as well as the most effective way(s) to combine SBRT with systemic therapy. Studies suggest that the occurrence of the abscopal effect (when radiation shrinks tumors distant from the area where the radiation was delivered) is rare and should not be relied upon.9 Instead, researchers should investigate the alternating high-dose radiation therapy for the initial tumor—to prime the immune system—with low-dose radiation therapy (known as the RadScopal technique) to visible metastases in the hope of triggering a broader immune response.12
In order to optimize and personalize the treatment of patients with oligometastases, new trials need to be performed using innovative designs, refined selection criteria, and novel clinical endpoints.9 No two patients have the same experience with cancer…thus their treatment should be tailored accordingly.
How could SCINTIX technology benefit patients with oligometastatic disease?
RefleXion’s SCINTIX® biology-guided radiotherapy, features a unique targeting and motion-management technology that could benefit patients at all stages of cancer progression, including oligometastatic disease. SCINTIX therapy, which uses the radiotracer FDG (fluorodeoxyglucose), received FDA clearance in February 2023 for lung and bone tumors. Lung and bone metastases are among the most common metastatic sites for many solid malignancies.
For treatment, a patient is injected with FDG before lying down—a radiotracer that combines a diagnostic radioisotope (fluorine-18) with glucose (sugar), which is consumed by cancer cells at a greater rate than healthy tissue. As the cancer cells consume the FDG, emissions are produced and stream live from the tumor. The RefleXion® X1 machine with SCINTIX technology uses these emissions from the patient’s cancer cells to then determine where to deliver radiation, second-by-second, during the actual treatment delivery.
SCINTIX technology detects emissions from the injected radiotracer and, in about half a second, sends beamlets of radiation directly to tumors to destroy them.
Using anatomic data from computed tomography (CT) and functional imaging data from PET to direct personalized radiotherapy, SCINTIX technology detects emissions from the injected radiotracer and, in about half a second, sends beamlets of radiation directly to tumors to destroy them—essentially turning the biological signature of cancer back on itself.
By tracking the delivery of the radiation dose to the cancer cells real-time, when the radiotherapy is occurring—like a spotlight that follows a tumor—SCINTIX is designed to eliminate the need for delivering high doses of radiation to the entire motion path of the target. Therefore, potentially more healthy tissue in the surrounding organ is spared from injury, resulting in less toxicity for the patient.
RefleXion X1 is the only dual-treatment modality radiotherapy platform.
In addition to SCINTIX therapy, the RefleXion X1 radiotherapy platform can perform intensity-modulated radiation therapy (IMRT), SBRT, and stereotactic radiosurgery (SRS).
The features and capabilities of the technology align with the latest published best practice guidelines for SBRT for lung oligometastases.13
Among others, the current best practice guidelines for SBRT for lung oligometastases include:
- FDG PET/CT and sequential PET images are recommended for accurate diagnosis and for identifying the stage of lung metastasis.
- Definitive local therapy is recommended for lung metastases.
- SBRT is recommended for oligometastases up to 5cm in diameter.
- Single fraction SBRT should be considered for peripheral lesions if distant from serial organs at risk.
- Use of motion management with 4DCT is recommended.
The fact that SCINTIX therapy uses PET imaging to monitor treatment delivery could also be helpful as it gives metabolic information on oligometastases. While not a diagnostic PET imaging system, measuring the metabolic tumor volume on the RefleXion X1 PET captured at the start of different treatment doses could provide vital prognostic information.
SCINTIX therapy, which can treat tumors up to 5cm in diameter, may be used to target multiple metastases sequentially in a single session. The RefleXion vision is to be able to treat multiple tumors simultaneously. There are legions of patients worldwide, many of whom have not succeeded with conventional radiation therapy techniques. SCINTIX therapy aims to change the balance for these patients.
Written by Dorine de Jong, PhD
References
- https://www.mdanderson.org/cancerwise/what-is-oligometastatic-cancer–what-patients-with-stage-iv-cancer-should-know.h00-159617067.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9873316/
- https://pubmed.ncbi.nlm.nih.gov/7799047/
- https://pubmed.ncbi.nlm.nih.gov/32205532/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8507821/
- https://pubmed.ncbi.nlm.nih.gov/31067138/
- https://pubmed.ncbi.nlm.nih.gov/30982687/
- https://pubmed.ncbi.nlm.nih.gov/35094066/
- https://pubmed.ncbi.nlm.nih.gov/36567069/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6699121/
- https://stanfordhealthcare.org/medical-treatments/s/stereotactic-body-radiation-therapy.html
- https://www.mdpi.com/2673-5601/3/1/6
- https://pubmed.ncbi.nlm.nih.gov/37390723/