People
Radiotherapy—A Bridge to Survival for Many Cancer Patients
April 20, 2022
Every patient’s cancer journey and care plan is unique. Oncologists factor in the stage of diagnosis, patient health and survivorship odds into a patient’s treatment options. Radiotherapy (also called radiation therapy) is one of three primary modalities used to treat cancer. Between half and two-thirds of cancer patients receive radiotherapy.1
Jill Feldman is a survivor of lung cancer and advocate. Her grandfather, father, aunt and mother were diagnosed with lung cancer and subsequently died from it. Jill has battled lung cancer for over a decade since her first diagnosis of Stage 1A lung cancer in 2009. Her cancer has progressed since her initial diagnosis into a chronic condition managed through multiple treatment approaches. “Although there wasn’t any research at the time for using SBRT2 for intrapulmonary metastases, we did it for three unruly cancers. It kept me off of systemic therapy for close to five years,” she says.
The American Cancer Society (ACS) defines radiotherapy as “the use of high-energy beams or particles to kill cancer cells and may be delivered from a source outside the body (as in external beam radiotherapy or EBRT) or placed internally (e.g., brachytherapy.)3 Radiotherapy may be the only treatment a cancer patient receives, or it might be used in combination with surgery, chemotherapy and/or immunotherapy. It may be used to treat or cure early-stage cancers, to prevent cancer from recurring somewhere else, to treat advanced-stage cancer symptoms or for palliative care.
When patients consider radiotherapy as a treatment option, they are likely concerned about short- (acute) and long-term (chronic) side effects. However, for many patients, the benefits of radiotherapy outweigh the potential side effects. For example, radiation therapy contributes to 40% of all cancer cures worldwide, and it reduces the risk of recurrence.5
Radiation therapy contributes to 40% of all cancer cures worldwide, and it reduces the risk of recurrence.
Although radiation has been used since 1896, there can still be a stigma associated with it. In 2010, The New York Times published a series of articles,6 which heightened concerns that radiotherapy is harmful and detrimental. The New York Times reporting prompted the American Society for Radiation Oncology and other radiotherapy associations to publish Safety Is No Accident: A Framework for Quality Radiation Oncology Care.7 Radiation oncologists, medical physicists and radiation therapists are highly trained experts who work diligently to ensure that radiotherapy treatments are safe for patients. Yet, some patients may still be concerned about the prolonged exposure to radiation that occurs with conventional radiotherapy as patients typically receive treatment in multiple sessions over the course of several weeks. Patients also worry about damage to healthy tissue surrounding the tumor and radiation impacting vital organs. For example, a breast cancer patient may worry about their heart and/or lungs being impacted by the radiotherapy treatments. According to the ACS, “Nearby normal cells can also be affected by radiation, but most recover and go back to working the way they should.”4
Advances in radiation physics and computer technology over the past several decades have helped the modality progress. Radiotherapy is more precise and is becoming more tailored to each patient. The precision comes in large part from the advanced capabilities to manage motion of the tumor and the patient effectively, which will reduce toxicity and lessen side effects. The ability to “see” the tumor also means less toxicity and fewer side effects.
In a recent op-ed appearing in the international journal, Lung Cancer, Feldman wrote that she was fortunate to receive SBRT (Stereotactic body Radiation Therapy). “SBRT was life-changing and life-saving for me. It played a critical role in managing the cancer, and it allowed me to prolong going back on systemic therapy, which gave research time to advance and develop new therapies,” she says.
“SBRT was life-changing and life-saving for me. It played a critical role in managing the cancer, and it allowed me to prolong going back on systemic therapy, which gave research time to advance and develop new therapies.”
Jill Feldman
Co-Founder of EGFR Resisters
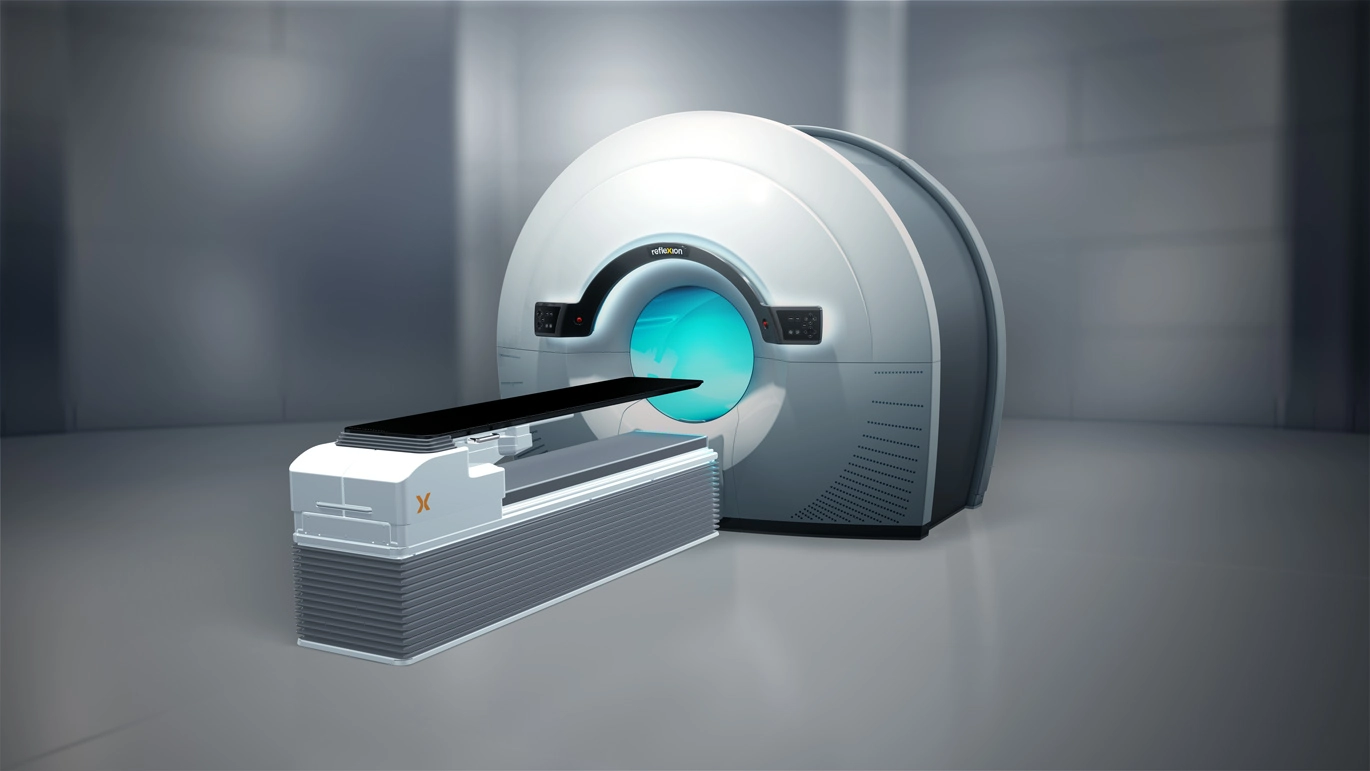
RefleXion’s biology-guided radiotherapy* (BgRT) is a new treatment modality that will one day offer precision and tailored treatment. It is the first and only technology to use injected radiotracers to produce active signals, called emissions, from each tumor to guide treatment delivery. The vision for BgRT is to expand treatment options for patients with all stages of cancer—a change from single tumor therapy to the ability to one day treat multiple tumors in the same treatment session in cancers that have metastasized.
Specifically, RefleXion’s X1 has the capability to combine PET (positron-emission tomography) imaging data with radiotherapy to enable tumors to continuously signal their location. The technology will use biological emissions from a patient’s cancer cells to guide the radiotherapy treatment, even to tumors that are moving – which will be a leap forward in the ongoing goal of managing motion, thereby potentially reducing margins, lowering toxicity and lessening side effects.
Radiotherapy has been used to treat cancer for more than 100 years. With all the technological advancements, it is, and will continue to be, a mainstay in the arsenal to treat cancer. Patients like Jill Feldman credit radiotherapy with still being alive today. “Radiotherapy was vital to my cancer treatment and survivorship,” she says.
*The RefleXion® X1 is cleared for SBRT/SRS/IMRT. BgRT is pending regulatory review and is not commercially available.
References:
- ASTRO. Access to radiation therapy has grown, especially in densely populated areas. 2022.
- Memorial Sloan Kettering Cancer Center. What Is SBRT? 2022.
- American Cancer Society. Cancer Treatment & Survivorship: Facts & Figures 2019-2021.
- American Cancer Society. How Radiation Therapy Is Used to Treat Cancer. 2022.
- Radiation Oncology Targeting Cancer. Benefits and Effectiveness. October 10, 2020.
- Bogdanich W. Radiation Offers New Cures, and Ways to Do Harm. The New York Times. January 23, 2010.
- American Society for Radiation Oncology. Safety Is No Accident: A Framework for Quality Radiation Oncology Care. 2019.